Utilization of Health Technology in Addressing Health Disparities
 |
| Sherine El-Toukhy, PhD, MA, NIH Distinguished Scholar, National Institute on Minority Health & Health Disparities |
The AHRQ publishes the National Healthcare Quality and Disparities Report annually to assess the performance of our healthcare system and disparities based on measures of quality and access. The report summarized that over 50% of measures that assessed access to healthcare from 2000 to 2017 showed improvement; 33% did not change and 14% showed worsening. Quality of care improved overall but pace of improvement varied with only 1/3rd of care coordination measures improving and care affordability not changing at all in this period. Health disparities persist, especially for poor and uninsured populations, with Blacks, American Indians and Alaska Natives, and Native
Hawaiians/Pacific Islanders receiving worse care than Whites for about
40% of quality measures. Clearly, we need to collectively make improvements in these important areas in how our nation's healthcare system(s) operate.
Our NAM panel explored these three major topics:
Health IT can advance our collective efforts to reduce health disparities by focusing on patient-centered care, promoting patient dignity and personal responsibility, and improving communicaitons among providers, patients, payers and the society at large.
Our NAM panel explored these three major topics:
- Will Health IT create a major transformation or just an incremental change? Chirs Gibbons, Distinguished Health IT Scholar at the FCC and CEO of the Greystone Group argued that Health IT has the power to improve Healthcare Quality and Disparities measures similar to how Railroads (1800-), telephone system (1920-), electricity grid (1930-), Radio & Television networks (1940-), interstate highways (1950-) and Broadband (1980-) transformed societies. These networks transformed societies because they enabled connections between people, good and services. We discussed opportunities across various healthcare domains that have the potential to be transformed through Health IT including but not limited to telemedicine, health literacy, disease surveillance and screening.
- SmokeFreeTxt program - Sherine El-Toukhy, Distinguished scholar at the The National Institute on Minority Health and Health Disparities discussed her team's work on an important application of Health IT in smoking cessation programs among different racial and ethnic groups. She and her colleagues compared Blacks (n=1333) and Whites (n=7154) in a TXT based smoking cessation program sponsored by the NCI and found that while Black smokers enrolled in the nationwide mobile smoking cessation program at rates comparable to White smokers, they were significantly less likely to engage with the program or quit smoking. We discussed the opportunity to examine social, cultural and technological barriers to cessation for Black smokers.
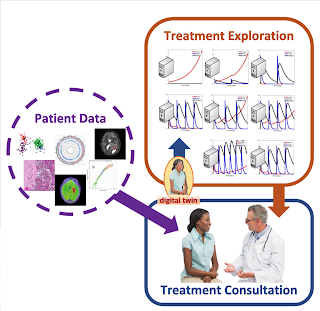
- Democratizing Precision Oncology - Could we bring a multi-disciplinary tumor board analysis to every patient with cancer irrespective of their access to tertiary care, academic cancer centers? Tumor boards currently involve assembling clinical cancer experts in one conference room, mostly during wee hours to avoid their patient care window, to discuss one or two complex cases with advanced, metastatic cancers. We recently published a study with 1725 cancer patients wherein a cloud-based, asynchronous HIT platform (developed by Perthera) was used by 200 clinical teams from academic health systems and community clinics across the United States to integrate data and reach consensus on treatment plans using a purpose-designed chat room. This Virtual Tumor Board platform, which does not require in-person meeting of clinicians, crunched the patient's molecular profile, medical history, and demographics and compared them to 51,000+ expert rules that included NCCN guidelines, FDA drug approval status, clinical trial eligibility and knowledgebases that linked genes to cancer types and appropriate drugs. This algorithm allowed for accurate matching of patients to clinical trials in the vicinity of patient's homes and reduced delivery time for patient reports from 14 to 4 days. We discussed future opportunities to understand uptake of such digital platforms among clinicians and patients in the context of health disparities.
Health IT can advance our collective efforts to reduce health disparities by focusing on patient-centered care, promoting patient dignity and personal responsibility, and improving communicaitons among providers, patients, payers and the society at large.

Comments
Post a Comment