Not all news about COVID-19 is bad - Part 4
Dear friends,
This is part 4 in my blogpost series titled "Not all news about COVID-19 is bad" where I attempt to capture scientifically-rigorous, evidence-based, and data-driven synthesis of promising news items and peer-reviewed articles relating to the COVID-19 global pandemic. My goal is to present topics in health care, life sciences and health IT in a simple language for anyone who may be interested. I prioritize current topics from medical/scientific literature and social media that overlap with the interests of folks in my personal and professional networks.
You can read part 1, part 2 and part 3 of this series here.
In today's post, I review two topics that were requested by some of you on how the COVID-19 pandemic might end and the race to a vaccine. In addition, I review some of the latest Artificial Intelligence tools that are poised to help with COVID-19.
1. How might COVID-19 pandemic come to an end? The island-nation of New Zealand declared that it has won the battle against COVID-19, at least for the present. As of this writing, the Johns Hopkins COVID-19 Dashboard shows 1,499 confirmed cases in NZ with 21 deaths. In NZ, new cases have come down drastically since April 5 and their director-general of health attributes this downward trend to aggressive contact tracing, the technology that uses bluetooth-enabled location services to track down anyone in recent contact with a newly diagnosed patient, then monitor the health of these contacts. We want similar downward trends in new cases and deaths for the whole world. While no one knows yet how this global pandemic will end, we can look at past pandemics for clues. The SARS-CoV-2 virus which causes COVID-19 is an RNA virus, meaning it has a single strand of genetic material packaged in a protein shell. When the virus comes in contact with a human cell, it makes new copies of itself and attacks other human cells. These viruses are constantly mutating or changing, so they are novel enough that the human immune system does not recognize them as foreign invaders and mark them for destruction. This is why large numbers of people get sick very quickly. Social contact and lack of effective anti-viral drugs make the situation worse. Let us examine how prior such pandemics ended. It usually takes many years to achieve herd immunity, where majority of the population have developed immunity against this virus and therefore cannot spread it to others anymore. This was the case with the H1N1 influenza pandemic 1918-1919 which infected 500 million people and killed 50-100 million. It took another strain of this virus, H2N2 to get rid of the older H1N1 viral strain from the world. Aggressive containment of infected people and their contacts helped the 2003 SARS epidemic, also caused by a Coronavirus (SARS-CoV). Containment worked so well in Hong Kong and Toronto that there were only 8,098 SARS cases globally and deaths were limited to 774 people. When a new H1N1 influenza virus appeared in 2009, scientists developed a vaccine for it within 6 months, since the biology of this virus was well-studies for many decades. COVID-19 will end with a combination of all these and other measures including contact tracing, social control measures, easy, at-home testing kits to detect the virus, antibody tests to detect who has already acquired immunity, rapid development of a potent vaccine to keep the population from contracting the disease and anti-viral drugs to ease symptoms in sick patients. As citizens, we can participate by educating ourselves about these measures, following social distancing guidelines and enrolling in clinical studies to help improve our understanding of this pandemic.
2. Vaccine will be ready to deploy in clinical trials this Fall. A vaccine for COVID-19 will be developed, there is no other alternative. Dr. Scott Gottlieb, former FDA chief and a key voice of leadership during the Pandemic, has said that millions of doses of vaccine for SARS-CoV-2 will be available for human clinical trials in the Fall. Multiple vaccine platforms are currently under development. DNA and RNA-based vaccine platforms offer maximum speed for developing a vaccine against COVID-19 compared to more traditional platforms such as live attenuated virus because they do not require prolonged cell culture and fermentation processes. But these platforms pose different challenges. Because they are new platforms, their safety has to be thoroughly tested before they can be given to humans. They also have to demonstrate a consistent immune response against the pathogen and be suitable for large-sale manufacturing to billions of doses. The virus's spike protein offers a promising immunogen as a vaccine platform, but the development will not be as fast as the DNA or RNA based platforms due to the extensive protein purification processes required. Exhibit 1 from an article in the New England Journal of Medicine shows various vaccines under development by different Pharmaceutical and Biotech firms. A more compete list of vaccines under development can be found at this World Health Organization website.
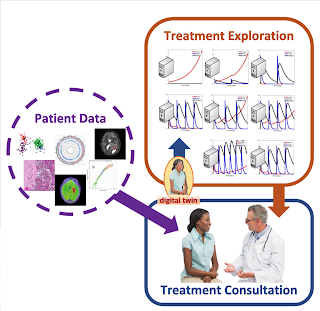
3. Artificial Intelligence provides new scientific insights. The availability of large/labeled datasets has prompted data scientists to apply Artificial intelligence and machine learning techniques to predict various outcomes that are useful in the COVID-19 pandemic. Here I cite a few examples - 1) BenevolentAI's Artificial Intelligence-derived knowledge graph enabled identification of a potential therapeutic agent that could be effective against SARS-CoV-2, the virus that causes COVID-19. This drug Baricitinib, already approved for use in patients with Rheumatoid arthritis, may help contain the strong inflammatory response (called the "cytokine storm") that develops in COVID-positive patients. AI algorithms are very good at identifying such candidate drugs, approved for other diseases, that can be repurposed for use in COVID-19 after extensive testing; 2) Case Western Reserve University researchers have developed an AI-based technique to identify which COVID-19 patients need ventilators and which ones don't. Using digital images from chest scans (Exhibit 2), they trained computers to accurately detect unique textural patterns that are not visible to human eye, combined them with other clinical features of the patient to accurately predict patient's ventilator needs in the ICU. This AI's prediction accuracy is between 68-75% and they hope to improve it by adding additional clinical and co-morbidity (other diseases in the patient) factors. When fully developed and deployed, such methods can be used to triage COVID patients to efficiently utilize hospital resources; and 3) Researchers at Lawrence Berkley National Labs have repurposed their Natural Language Processing tool which mines millions of articles in literature within seconds to find connections that may not be otherwise apparent for COVID-19. This tool called COVIDScholar was developed in response to the March call for action by the US White House Office of Science and Technology Policy. Since we are developing a study to explore "cytokine storm" in patients with COVID-19 at the Georgetown University Medical Center, I searched for this phrase in COVIDScholar which resulted in 9035 matches from published literature. Then I filtered for COVID-19 related results which resulted in 833 matches; then setting filters for peer-reviewed only, diagnostics related literature published in 2020, I ended up with one paper that matched my search criteria 100%. This complete search and filtering process took ~5 seconds and saved me a lot of time from scanning 100's of articles of interest for COVID-19 cytokine storm. Indeed, we are learning new ways of how work happens during the COVID-19 pandemic.
Some final thoughts
I welcome you to read about Georgetown University Medical Center's (disclosure: I work here) swift response to COVID-19 including updates on our work in supporting response in Africa, development of COVID-19 frontline guide for local governments to help protect their communities from the pandemic, and a novel clinical trial in cancer patients who are susceptible to COVID-19 and much more.
Published on May 14, 2020 in the highly reputed journal Health Affairs, this study estimates that without the Shelter-in-place and social distancing policies over the past two months, there would have been 10M COVID cases in the US by now, instead of the 1M that actually occurred.
Flattening the curve, COVID-19 data challenge has announced its winners. The winning entry was from COVID-19 Primer which helps users understand the scientific progress in the fight against COVID-19. Powered by NLP, you can read summaries and discover trends in the latest research papers on COVID-19. This is updated every 24 hours to keep up with ~200 new journal articles being published every day on COVID-19 related topics.
Finally, in related news, I am delighted to share that our Georgetown-Howard Universities Center for Clinical Translational Science (GHUCCTS) CTSA grant was renewed for the third cycle for five more years by the NCATS enabling continued research in "Discovery through Diversity". Key collaborators include the Medstar Health Research Institute, Washington DC VA Medical Center and Oak Ridge National Labs. Much of our work in GHUCCTS has been redirected to support COVID-19 research since March, 2020.
Together, we will beat COVID-19!
Thank you for reading and sharing.



Comments
Post a Comment